- Home
- Products
FHIR Data Exchange
Ezovion FHIR engine enables health data exchange between healthcare stakeholders.

Digital Healthcare Platform
Integrated healthcare ecosystem for patient-centric healthcare delivery.

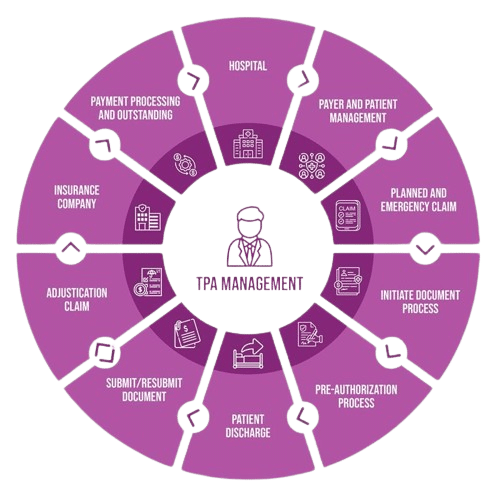
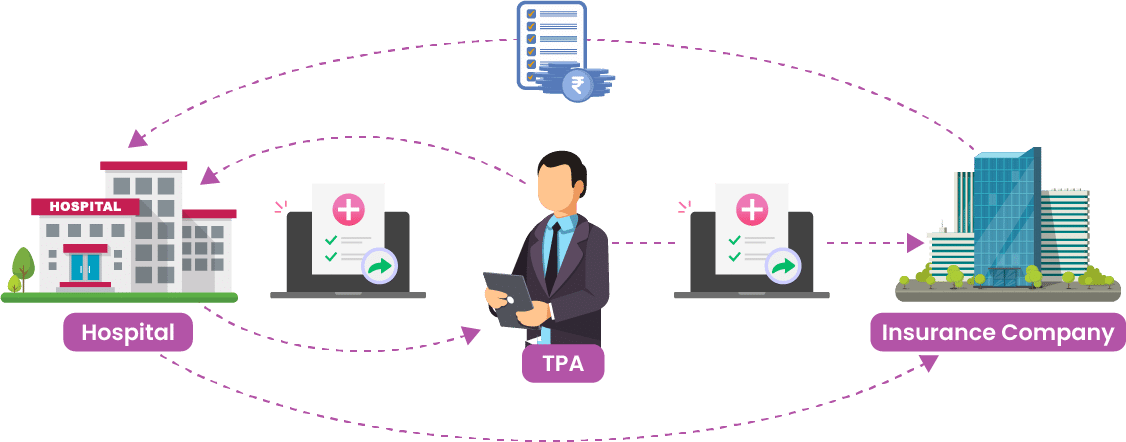
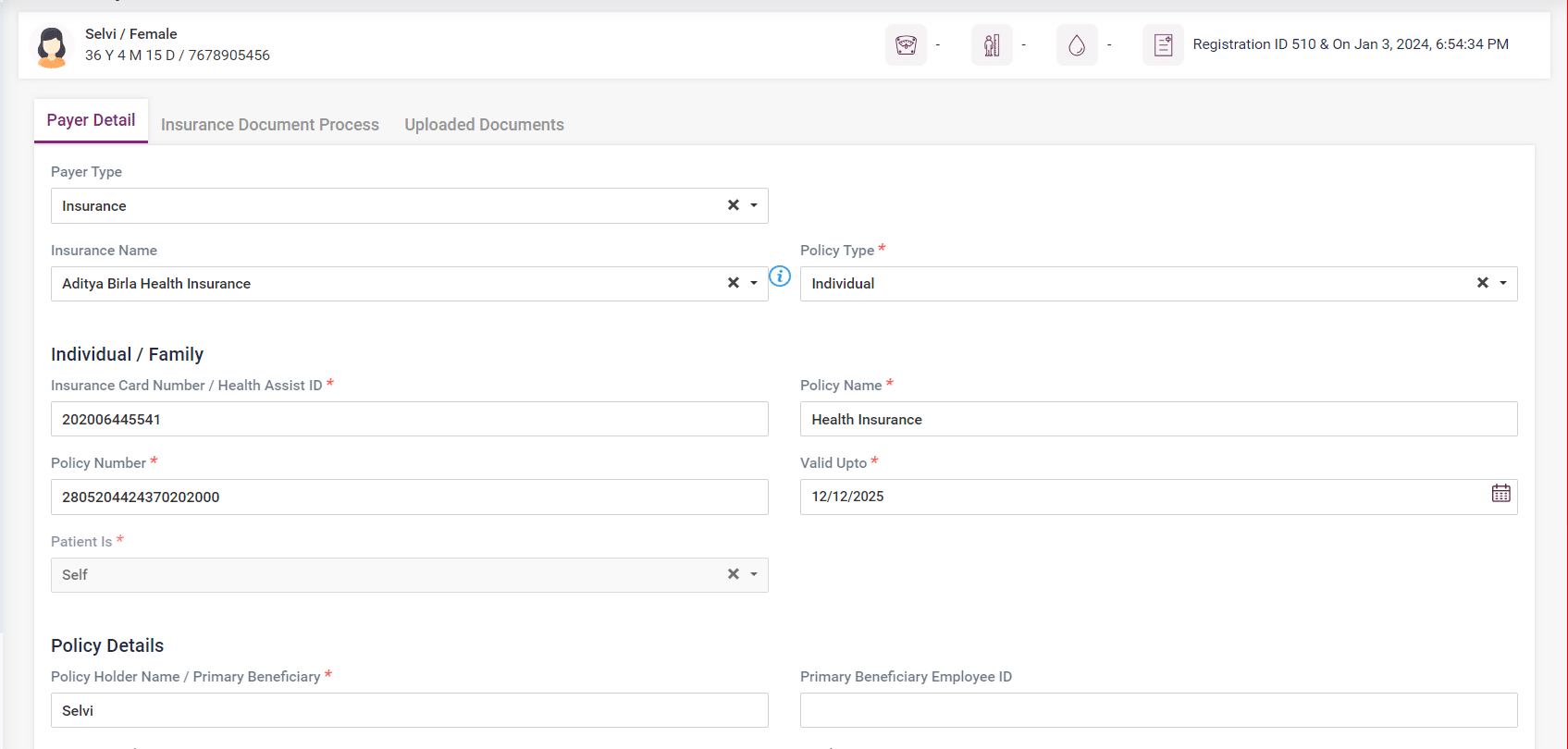
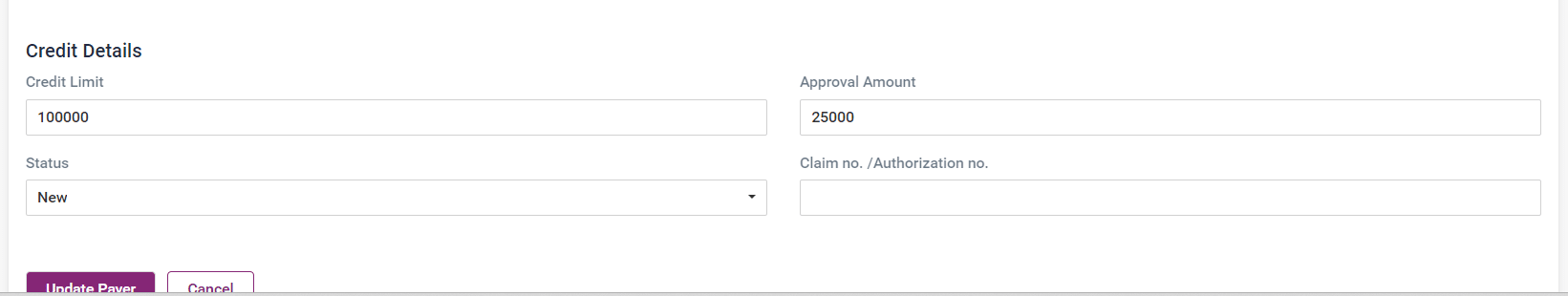
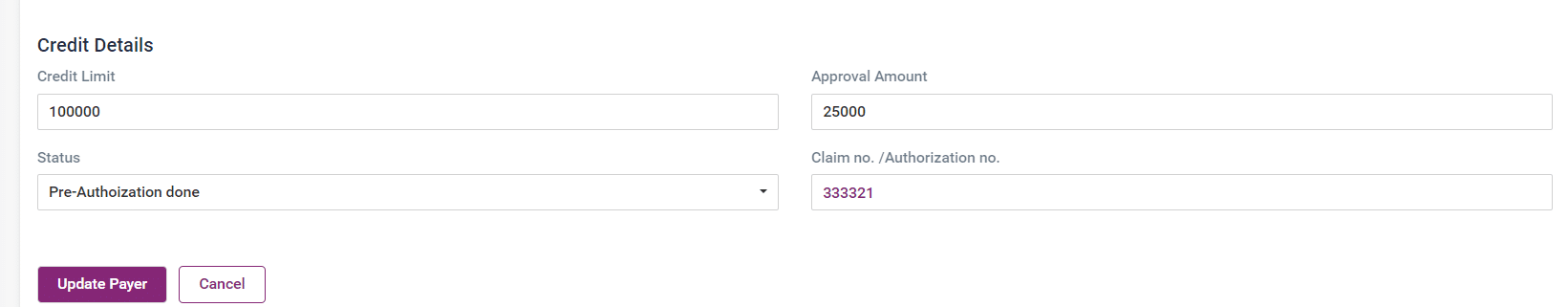
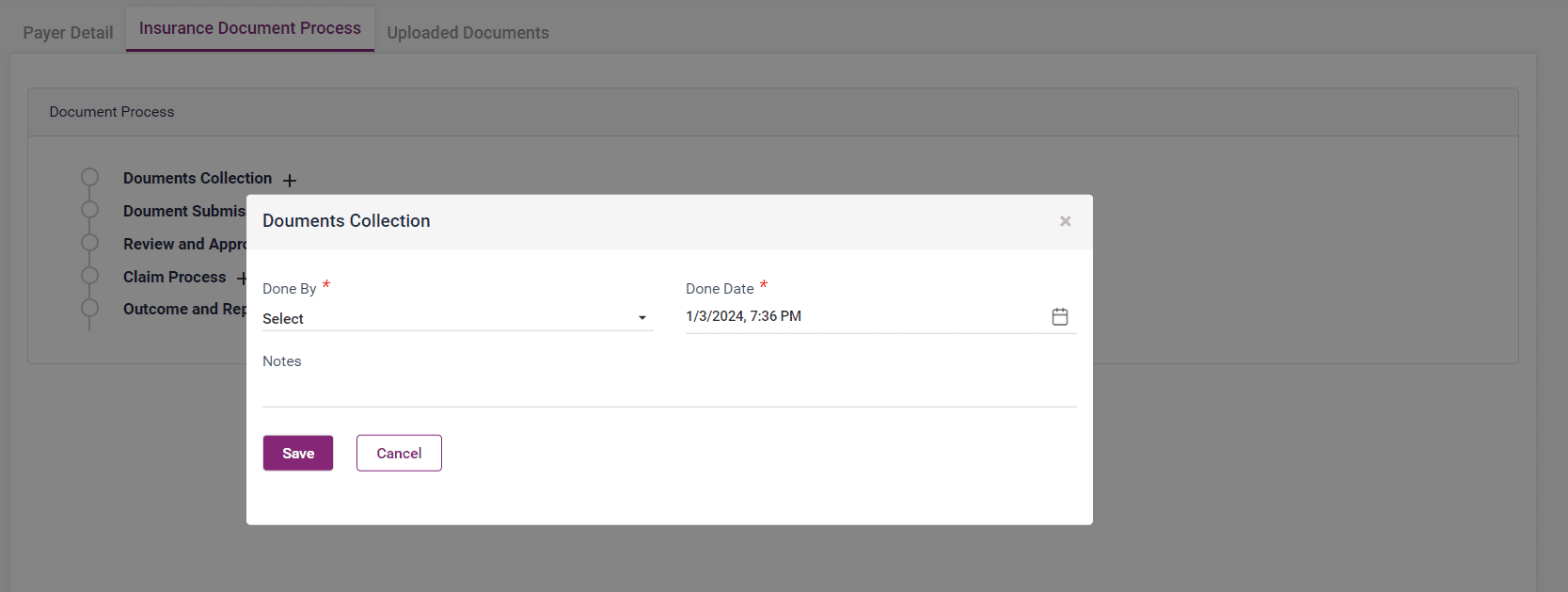
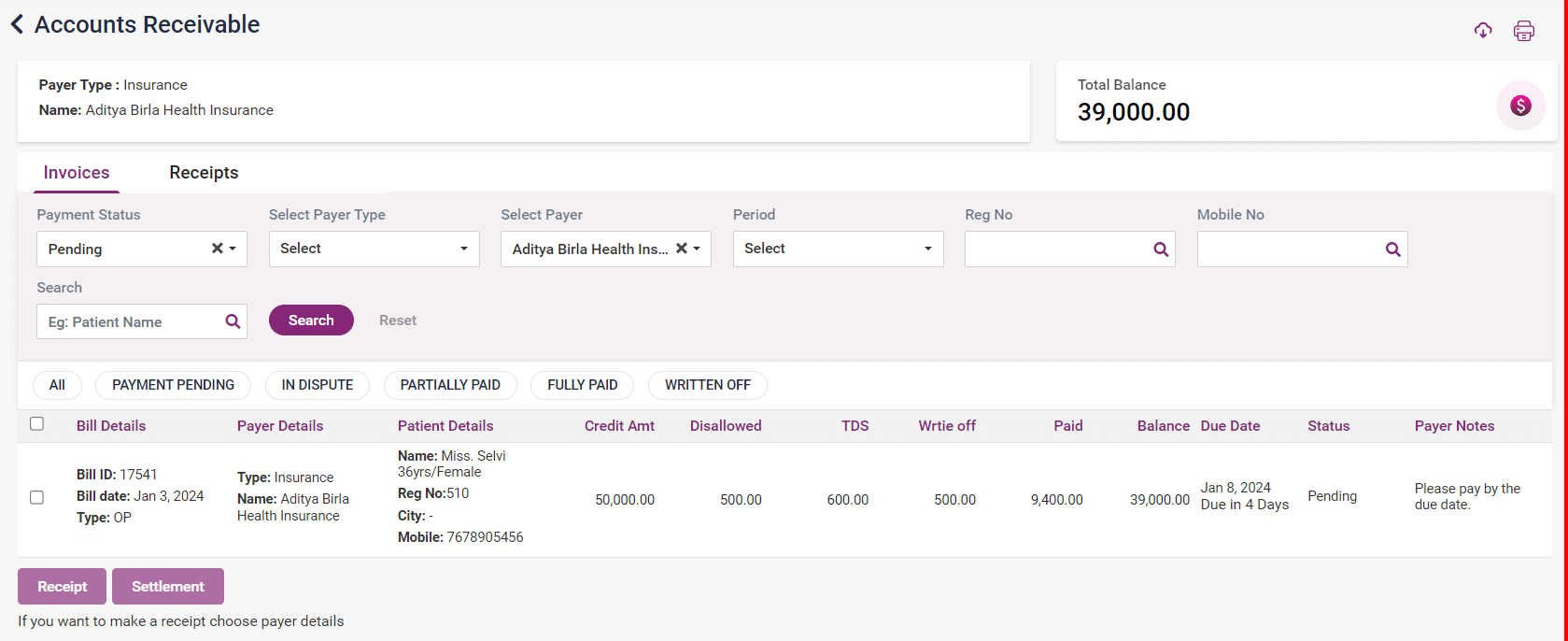
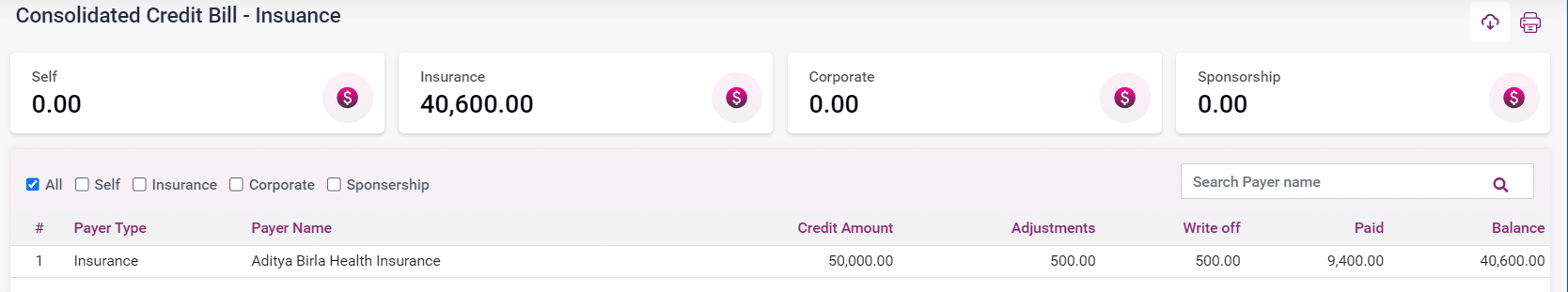
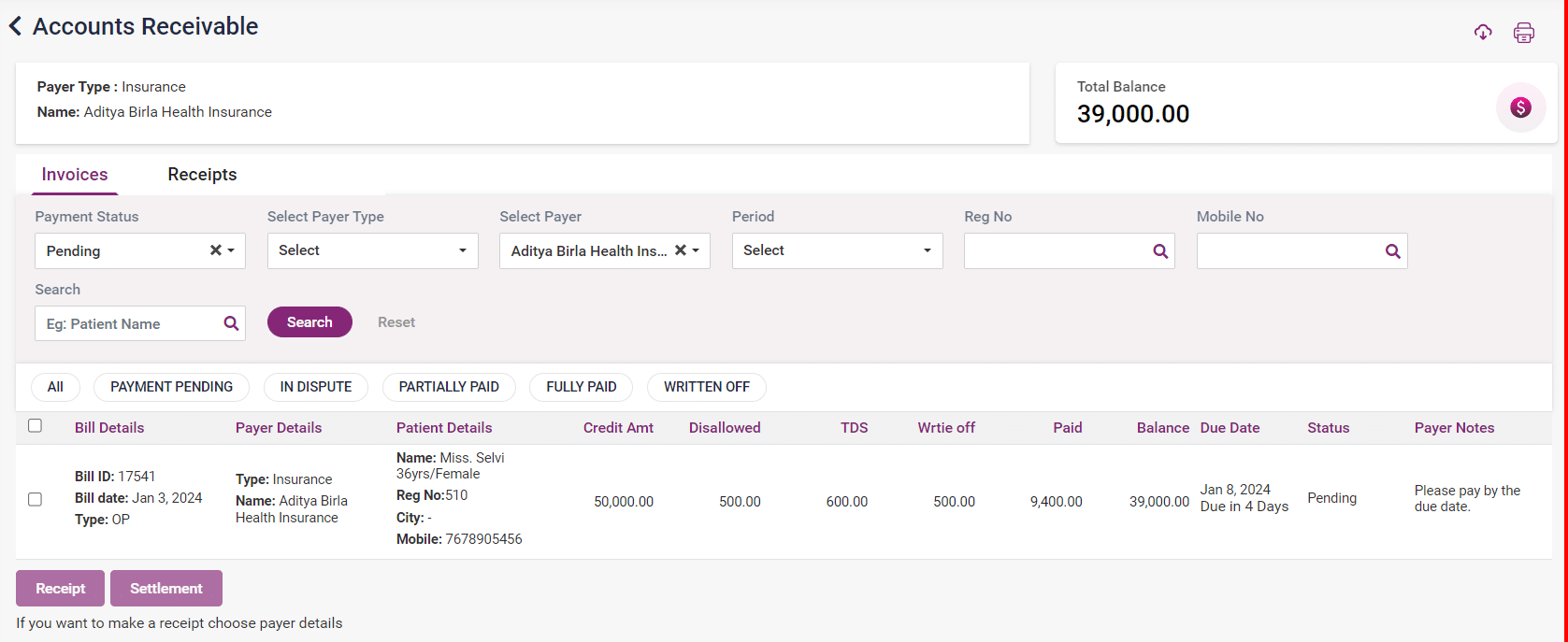
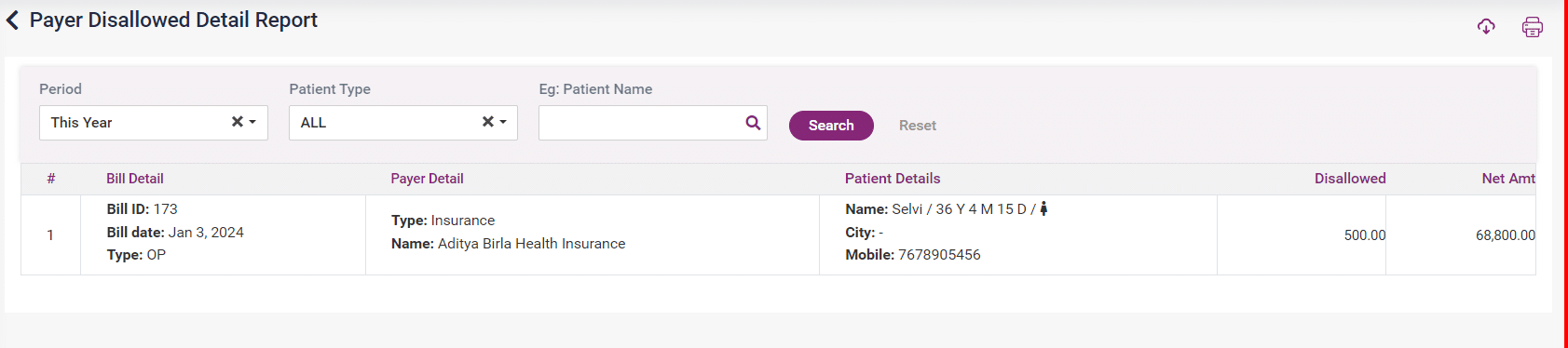
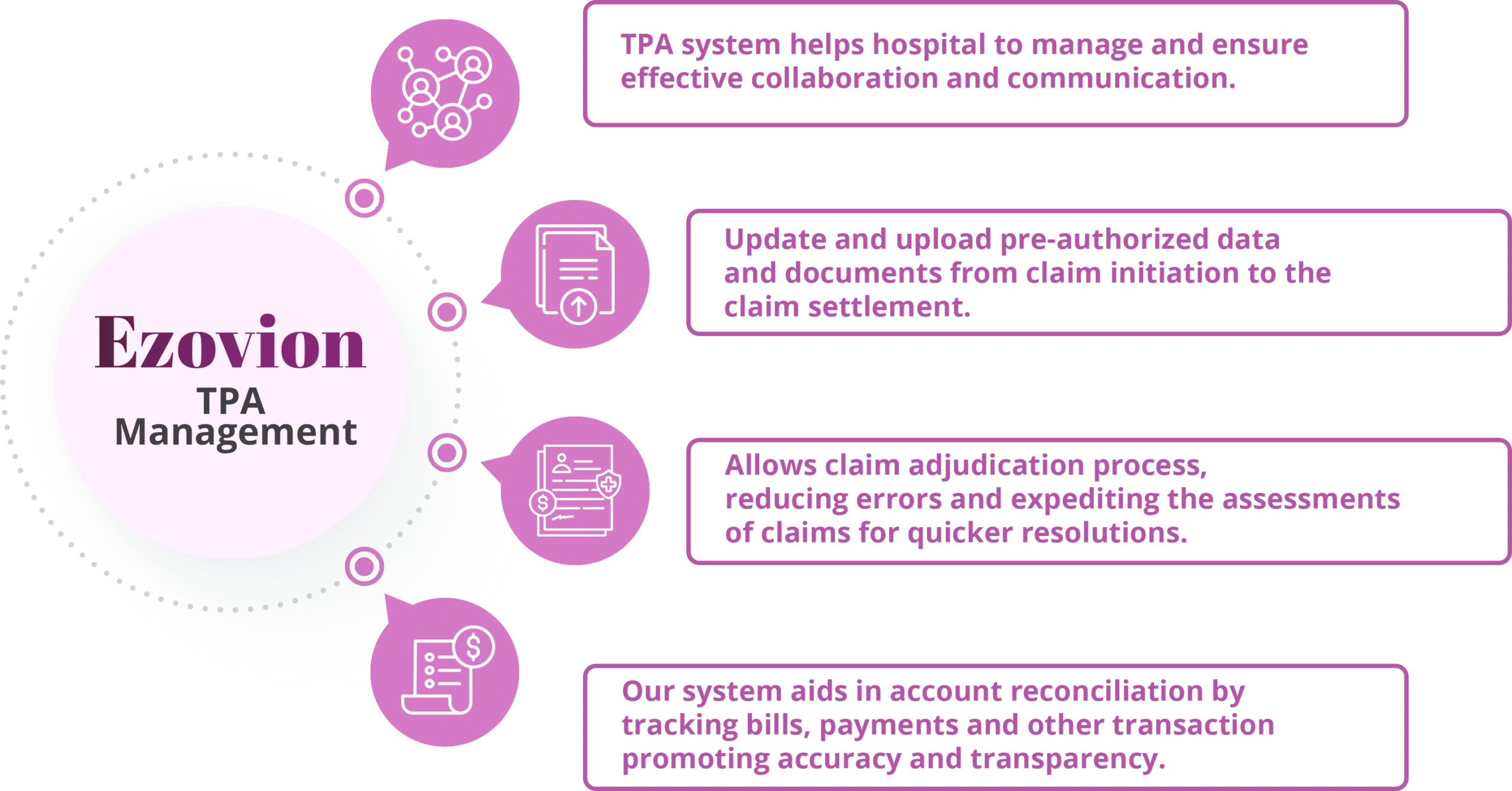
Revenue Cycle Management
Accelerate claim processing for faster account receivables.
- Services
- About Us